


Diễn Đàn Cựu Sinh Viên Quân Y
© 2010
© 2010
Fat, Full of Insulin and Forgetful
Loading
Pham H. Liem, MD
I have been studying Alzheimer's disease for 30 years and the nature of Alzheimer's has changed from a predominantly genetic based disorder to a predominantly metabolic based disorder. Many of us are having the problem without knowing it and by the time that all the symptoms become apparent, it will be too late to stop it. That's why I'd like to share my finding with you, so all of us can take appropriate measures to protect ourselves.
In the 1970's and 80's, Alzheimer's dementia accounted for 55-60% of all dementia in old age (over 65yo), 5-7% of cases are autosomal dominant genetic disorders PS1 and PS2 which cause over production of beta-amyloid causing neuritic plaques, 1-2 % have mutation of Amyloid Precursor Protein gene on chromosome 21, Down's syndrome also have excess beta amyloid. A major risk gene was identified, APO E4, 20% of the population have the gene while over 40% of Alzheimer's patients carry APO E4. 20-25% of dementia at that time was vascular dementia (arterio-sclerotic of cerebral vessels and mini strokes).
But, gradually over the 1990s, autopsy from brain banks beginning to report more and more Alzheimer's and Mixed (Alzheimer's+ Vascular dementia) so by 2009, Alzheimer's is the cause of over 80% of dementia in old age. Back in the 1980, a Canadian neurologist, Dr. Hachinski, using Xenon wash out technique, was able to come up with Hachinski Ischemia Scale as a clinical tool using vascular risk factors like hypertension, hypercholesterolemia and neurological symptoms of TIA and stroke to accurately distinguish Vascular dementia from Alzheimer's disease. Alas, over the years, all the vascular risk factors became risk factors for Alzheimer's disease as well. The question is Why? What happened?
In the late 1980s, the UAMS group identified inflammation like phenomenon in the brain of Alzheimer's with microglia acting as macrophage in the peripheral system, we demonstrated the presence of cytokines like IL1, IL6 and TNF alpha in and around the plaques but attempts to treat Alzheimer's with anti-inflammatory drugs only met with limited success and it never last long.
Several events happened since 2004- 2005 led to better understanding of the situation: First the Harvard group demonstrated that in patients with type 2 DM and therefore have hyperinsulinemia, the insulin degrading enzyme (IDE) which in the CNS is used to breakdown the beta amyloid got used up so more beta amyloid precipitate as Alzheimer's lesion. Then the University of Washington group demonstrated that the Alzheimer's neurons, particularly in the synapses, have problem process insulin signal, they are insulin resistant, some mistakenly called it type 3 DM. These conditions was initiated by inflammation and in turn worsen the inflammation.
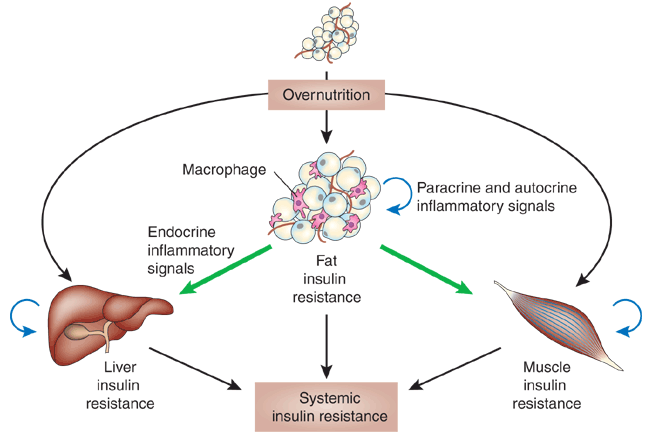
Around this time, the mechanism of Type 2 Insulin Resistant Diabetes became better understood; no longer should we be obsessed with blood glucose control but rather we should manage it the context of a metabolic disorder of Hypertension+Hyperlipidemia+Hyperinsulinemia from overactive and inflamed fat cells, particularly the visceral fat in the abdomen.
In fact, treating hypercholesterolemia with statin drug is helpful for the blood vessels, heart and kidneys but also lower the risk for Alzheimer's. Likewise treating hypertension with ACE Inhibitor is protective but only CNS active ACE I (Lisinopril, Fosinopril, Ramnipril) will also lower incidence of Alzheimer's. Metformin is the only helpful antidiabetic for the type 2 DM because it makes the insulin receptors more sensitive to insulin and patient lose weight while taking it. Many people have such good pancreas that we may have insulin resistance already but our glucose and HGb A1C are normal, of course we have hyperinsulinemia and inflammation with all the bad implications but will not know it until our pancreas is exhausted and we finally become hyperglycemic and was at last diagnosed with "diabetes" while the damage has been done. The statin and ACE I keep us living longer until the Alzheimer's synaptic dysfunction becomes apparent.
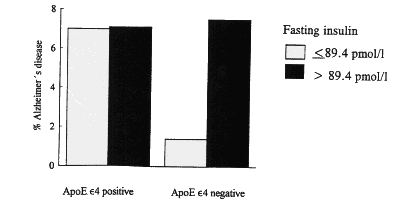
Hyperinsulinemia has become a stronger risk factor for Alzheimer's than APO E4.
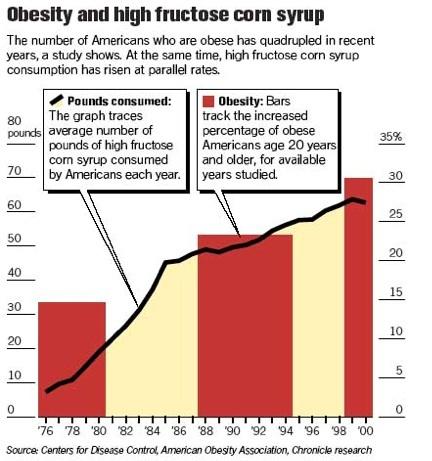
The USA has been and now most of the world is in an epidemic of obesity. In the 1970s and 80s, 20% of adult are obese (BMI>30) but now, in city like Houston the obesity rate is over 50%. Why? We blame automobile, TV and fast food but all of those have been around for over 50 years. What about video game? But how is that more sedentary than reading books? Actually the rate of obesity in the USA is closely matched with the introduction of High Fructose Sweetener in the food and beverages.
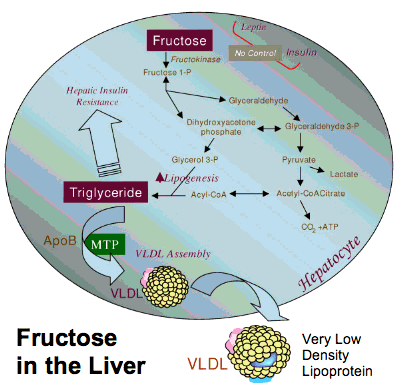
In the 1950s, 60s and 70s, adiposity and free fatty acids, hypercholesterolemia were results of consuming bad fat (saturated fats, mostly from animal sources) whereas today's metabolic problems are the results of consuming too much fructose. Unlike glucose metabolism in the liver to produce glycogen and also makes fat cells raise the level of leptin so you will feel full and eat less. Fructose will generate free fatty acids and have no effect on leptin level so you still feel hungry, a dangerous combination.
Free fatty acids promote inflammation, this combination results in insulin resistance, hyperinsulinemia and further fat cells dysfunction. They are the culprits of Metabolic Syndrome which is detrimental to many end organs such as heart, blood vessels, kidneys. In the brain, it can cause both Alzheimer's and Cerebro-vascular disease.
To prevent this, we should:
1- Watch our calories intake
2- Eat high protein, low fat diet.
3- Avoid food and beverage contain fructose (sweetened by HFCS or Apple Juice concentrate). Limit fructose source to fresh fruits only.
4- Maintain physical exercise (to elevate the level of neurotrophic factor).
5- Take statin (it's not just for cholesterol anymore)
6- Use CNS active ACE inhibitor as first line anti-hypertensive.
7- If you have hyperlipidemia, hypertension and have trouble trying to lose weight despite diet and exercise, check your fasting insulin level regardless of glucose status.
8- Take metformin to treat hyperinsulinemia, take B12 supplement because long term metformin intake can result in B12 deficiency.
9- Maintain a good level of 25 OH vitamin D, take supplement if necessary.
10- Consider adding Omega 3 Fatty Acid if statin and exercise does not give you good enough lipid profiles.
I have been studying Alzheimer's disease for 30 years and the nature of Alzheimer's has changed from a predominantly genetic based disorder to a predominantly metabolic based disorder. Many of us are having the problem without knowing it and by the time that all the symptoms become apparent, it will be too late to stop it. That's why I'd like to share my finding with you, so all of us can take appropriate measures to protect ourselves.
In the 1970's and 80's, Alzheimer's dementia accounted for 55-60% of all dementia in old age (over 65yo), 5-7% of cases are autosomal dominant genetic disorders PS1 and PS2 which cause over production of beta-amyloid causing neuritic plaques, 1-2 % have mutation of Amyloid Precursor Protein gene on chromosome 21, Down's syndrome also have excess beta amyloid. A major risk gene was identified, APO E4, 20% of the population have the gene while over 40% of Alzheimer's patients carry APO E4. 20-25% of dementia at that time was vascular dementia (arterio-sclerotic of cerebral vessels and mini strokes).
But, gradually over the 1990s, autopsy from brain banks beginning to report more and more Alzheimer's and Mixed (Alzheimer's+ Vascular dementia) so by 2009, Alzheimer's is the cause of over 80% of dementia in old age. Back in the 1980, a Canadian neurologist, Dr. Hachinski, using Xenon wash out technique, was able to come up with Hachinski Ischemia Scale as a clinical tool using vascular risk factors like hypertension, hypercholesterolemia and neurological symptoms of TIA and stroke to accurately distinguish Vascular dementia from Alzheimer's disease. Alas, over the years, all the vascular risk factors became risk factors for Alzheimer's disease as well. The question is Why? What happened?
In the late 1980s, the UAMS group identified inflammation like phenomenon in the brain of Alzheimer's with microglia acting as macrophage in the peripheral system, we demonstrated the presence of cytokines like IL1, IL6 and TNF alpha in and around the plaques but attempts to treat Alzheimer's with anti-inflammatory drugs only met with limited success and it never last long.
Several events happened since 2004- 2005 led to better understanding of the situation: First the Harvard group demonstrated that in patients with type 2 DM and therefore have hyperinsulinemia, the insulin degrading enzyme (IDE) which in the CNS is used to breakdown the beta amyloid got used up so more beta amyloid precipitate as Alzheimer's lesion. Then the University of Washington group demonstrated that the Alzheimer's neurons, particularly in the synapses, have problem process insulin signal, they are insulin resistant, some mistakenly called it type 3 DM. These conditions was initiated by inflammation and in turn worsen the inflammation.
Around this time, the mechanism of Type 2 Insulin Resistant Diabetes became better understood; no longer should we be obsessed with blood glucose control but rather we should manage it the context of a metabolic disorder of Hypertension+Hyperlipidemia+Hyperinsulinemia from overactive and inflamed fat cells, particularly the visceral fat in the abdomen.
In fact, treating hypercholesterolemia with statin drug is helpful for the blood vessels, heart and kidneys but also lower the risk for Alzheimer's. Likewise treating hypertension with ACE Inhibitor is protective but only CNS active ACE I (Lisinopril, Fosinopril, Ramnipril) will also lower incidence of Alzheimer's. Metformin is the only helpful antidiabetic for the type 2 DM because it makes the insulin receptors more sensitive to insulin and patient lose weight while taking it. Many people have such good pancreas that we may have insulin resistance already but our glucose and HGb A1C are normal, of course we have hyperinsulinemia and inflammation with all the bad implications but will not know it until our pancreas is exhausted and we finally become hyperglycemic and was at last diagnosed with "diabetes" while the damage has been done. The statin and ACE I keep us living longer until the Alzheimer's synaptic dysfunction becomes apparent.
Hyperinsulinemia has become a stronger risk factor for Alzheimer's than APO E4.
The USA has been and now most of the world is in an epidemic of obesity. In the 1970s and 80s, 20% of adult are obese (BMI>30) but now, in city like Houston the obesity rate is over 50%. Why? We blame automobile, TV and fast food but all of those have been around for over 50 years. What about video game? But how is that more sedentary than reading books? Actually the rate of obesity in the USA is closely matched with the introduction of High Fructose Sweetener in the food and beverages.
In the 1950s, 60s and 70s, adiposity and free fatty acids, hypercholesterolemia were results of consuming bad fat (saturated fats, mostly from animal sources) whereas today's metabolic problems are the results of consuming too much fructose. Unlike glucose metabolism in the liver to produce glycogen and also makes fat cells raise the level of leptin so you will feel full and eat less. Fructose will generate free fatty acids and have no effect on leptin level so you still feel hungry, a dangerous combination.
Free fatty acids promote inflammation, this combination results in insulin resistance, hyperinsulinemia and further fat cells dysfunction. They are the culprits of Metabolic Syndrome which is detrimental to many end organs such as heart, blood vessels, kidneys. In the brain, it can cause both Alzheimer's and Cerebro-vascular disease.
To prevent this, we should:
1- Watch our calories intake
2- Eat high protein, low fat diet.
3- Avoid food and beverage contain fructose (sweetened by HFCS or Apple Juice concentrate). Limit fructose source to fresh fruits only.
4- Maintain physical exercise (to elevate the level of neurotrophic factor).
5- Take statin (it's not just for cholesterol anymore)
6- Use CNS active ACE inhibitor as first line anti-hypertensive.
7- If you have hyperlipidemia, hypertension and have trouble trying to lose weight despite diet and exercise, check your fasting insulin level regardless of glucose status.
8- Take metformin to treat hyperinsulinemia, take B12 supplement because long term metformin intake can result in B12 deficiency.
9- Maintain a good level of 25 OH vitamin D, take supplement if necessary.
10- Consider adding Omega 3 Fatty Acid if statin and exercise does not give you good enough lipid profiles.
Click on for larger images below

.jpg)
.jpg)